NHS Wait Time Estimator
Estimate Your NHS Wait Time
Based on article analysis of NHS systemic challenges including staff shortages, funding gaps, and pandemic backlogs.
Every year, millions of people in the UK wait months for routine surgeries, specialist appointments, or even emergency care. You might have heard someone say, "I’ve been waiting over a year for my knee scan," or "My GP said they can’t fit me in until next summer." These aren’t isolated stories-they’re the new normal. But why does this keep happening? The NHS isn’t broken because of lazy staff or bad management. The reasons are deeper, older, and more structural than most people realize.
More people need care than ever before
The UK population is growing older. In 2026, over 19% of people are 65 or older-that’s up from 16% in 2010. Older adults need more medical care. They’re more likely to have arthritis, heart disease, diabetes, or cancer. A 70-year-old might see five different specialists in a year. A 30-year-old? Maybe once, if they’re lucky.
At the same time, chronic conditions are rising. Type 2 diabetes, obesity, and long COVID have exploded since 2020. These aren’t one-off visits. They require ongoing monitoring, medication adjustments, and regular check-ups. The NHS is now managing far more complex cases than it did 20 years ago. And the system hasn’t scaled up to match.
Funding hasn’t kept up with demand
The NHS budget grew by 3.5% annually between 2010 and 2020. That sounds good-until you realize inflation averaged 3.8% over the same period. When you adjust for rising costs, the NHS lost real spending power. Staff wages, medical supplies, and hospital maintenance all cost more. But the money didn’t rise fast enough.
By 2025, the NHS was spending £174 billion. Sounds huge? It is. But that’s £3,200 per person in the UK. Compare that to Germany, which spends £4,100 per person, or France at £4,300. The UK spends less per capita than most wealthy European countries. And when you factor in population growth and aging, that gap becomes a chasm.
Staff shortages are crippling the system
There are over 100,000 unfilled NHS jobs right now. Nurses, radiologists, physiotherapists, paramedics-you name it, they’re short. Why? Pay hasn’t kept pace. A nurse starting in 2025 earns £31,000. In 2010, that same job paid £28,000. Adjusted for inflation, that’s a 12% pay cut over 15 years.
Many left the profession. Others never joined. Training takes years. A doctor needs five years of medical school, two years of foundation training, then another four to six years to specialize. You can’t just hire more overnight. Meanwhile, burnout is common. One in three NHS workers says they’ve thought about quitting in the past year.

Backlogs from the pandemic never cleared
In 2020, the NHS postponed 4.5 million non-emergency procedures to make room for COVID-19 patients. At the time, it was necessary. But the backlog didn’t vanish when the pandemic ended. Hospitals didn’t get extra funding to catch up. Staff were exhausted. Equipment was outdated. Waiting lists kept growing.
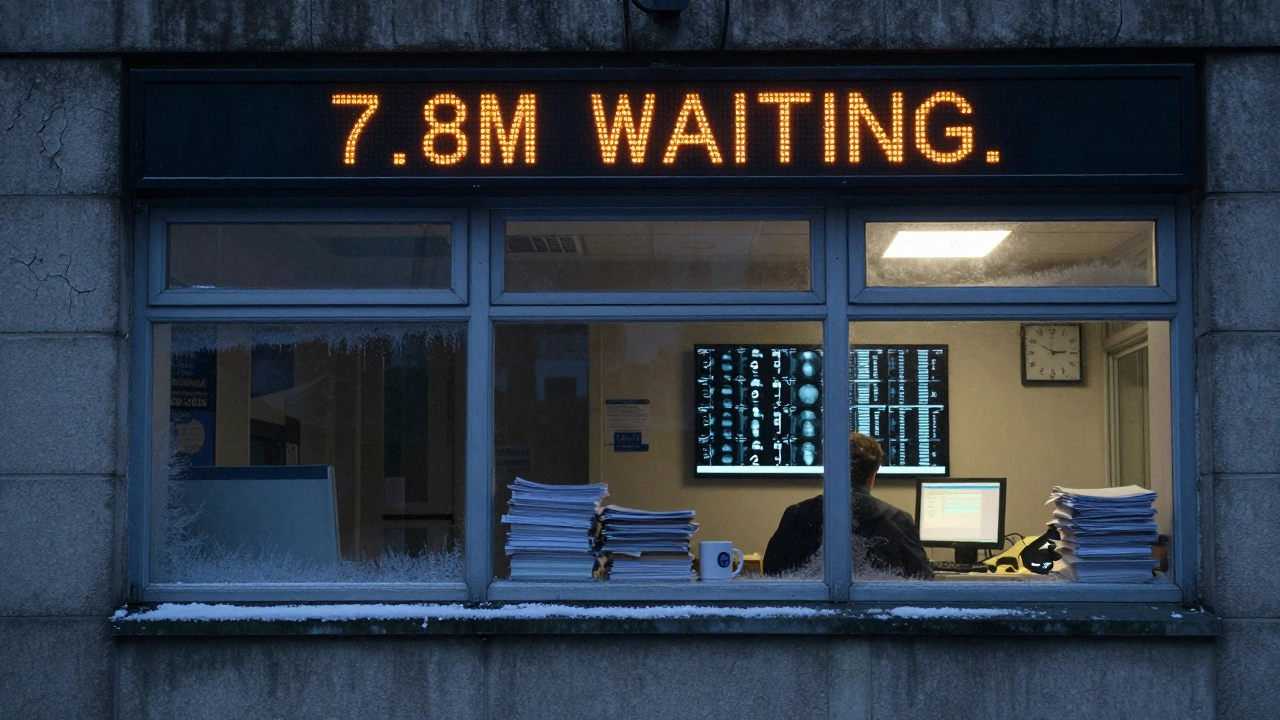
By 2026, over 7.8 million people were waiting for treatment. That’s more than the population of Scotland. Of those, 1.2 million have waited over a year. Some have waited two. And the system still doesn’t have the capacity to clear even half of that backlog in the next 12 months.
The system is built for a different time
The NHS was created in 1948. Its design assumes you go to your local hospital, get seen, and leave. But today, care is more complex. Patients often need scans, blood tests, specialist opinions, and follow-ups-all across different departments. Each step adds days or weeks.
Many hospitals still use paper records. Others have digital systems that don’t talk to each other. A GP might send a referral. The hospital receives it. But if the patient’s allergy history is in a different system, the appointment gets delayed. It’s like trying to build a car with parts from three different factories that don’t share blueprints.
Even scheduling is outdated. Many clinics still use phone-based booking. No online portals. No automated reminders. Patients miss appointments because they didn’t get a text. Those missed slots mean fewer people get seen the next day. It’s a cycle.
Private care isn’t the answer-it’s part of the problem
You might think, "Why don’t they just use private hospitals?" The truth is, they already do. The NHS pays private providers to handle overflow. In 2025, over 1.3 million NHS-funded procedures were done in private clinics.
But here’s the catch: private hospitals don’t work for free. They charge the NHS more per procedure than NHS hospitals do. So the NHS spends extra money to clear its own backlog. And private hospitals prioritize paying patients. That means NHS-funded patients often wait longer than private ones. It’s a band-aid that’s making the wound worse.
What’s being done? Not enough
The government has launched several initiatives. "Rapid diagnostic centres" to speed up cancer checks. "Community hubs" to handle minor issues outside hospitals. But these are small. They don’t fix the core issues: too few staff, too little funding, too much demand.
Some hospitals are trying digital triage. Chatbots that ask patients questions before they book an appointment. It helps filter out minor issues. But it doesn’t solve the specialist shortage. If there’s no endocrinologist to see you after the bot says "go here," you’re still stuck.
There’s no magic fix. More money? Yes. More staff? Absolutely. But those take time. And right now, the system is running on fumes.
What can you do?
If you’re waiting, know this: you’re not alone. And you’re not being ignored. The system is overwhelmed. But there are small steps you can take.
- Ask your GP for a referral to a different hospital. Some have shorter waits.
- Check if your condition qualifies for urgent care. Some backlogs are prioritized by clinical need.
- Use NHS 111 online. It can sometimes fast-track you.
- If you’re eligible, consider private options-but know you’re paying to jump a queue that’s still full.
The NHS isn’t failing because of bad people. It’s failing because the world changed, and the system didn’t change with it. Fixing it won’t be cheap. But it will be necessary.
Why are NHS waiting lists longer than in other countries?
The NHS serves a population of 67 million with less funding per person than most European countries. Germany, France, and Sweden spend 20-30% more per capita on healthcare. They also have fewer people per doctor. The UK has 2.8 doctors per 1,000 people. Germany has 4.3. That gap means longer waits for appointments, scans, and surgeries.
Is the NHS underfunded compared to its historical budget?
In real terms, yes. Between 2010 and 2020, NHS funding rose by 3.5% per year, but inflation was 3.8%. That means the NHS lost buying power. Staff wages, medicines, and equipment costs rose faster than the budget. By 2025, the NHS had less real funding than it did in 2010 when adjusted for inflation and population growth.
Do private hospitals help reduce NHS wait times?
They help a little, but not enough. The NHS pays private clinics to treat patients, but those clinics charge more than NHS hospitals. This drains NHS funds without solving the root problem. Plus, private hospitals prioritize patients who pay directly. NHS-funded patients often wait longer in private clinics than they would in NHS ones.
Why can’t the NHS just hire more staff?
Training doctors and nurses takes years. Medical school is five years, followed by two years of foundation training and up to six more for specialization. Even if they started hiring today, it would take 8-10 years to fill the current gap. Meanwhile, burnout and low pay are pushing existing staff out faster than new ones can join.
Are waiting times getting worse every year?
Yes. In 2019, 4.2 million people were waiting for treatment. By 2026, that number had jumped to 7.8 million. The pandemic pushed it higher, but the trend was already growing. The number of people waiting over a year has tripled since 2019. Without major changes, it will keep rising.