Back Pain Medication Risk Assessment Tool
Understanding Pain Medication Risks
The strongest medication isn't always the best choice. This tool helps you understand how your medical history affects your suitability for strong pain medications, based on current medical guidelines.
Note: This is not medical advice. Always consult your doctor before making any changes to your pain management plan.
Tell us about your pain and medical history
Severe back pain isn’t just uncomfortable-it can stop you from sleeping, working, or even standing up straight. When over-the-counter painkillers like ibuprofen or paracetamol don’t touch the pain, doctors often turn to stronger medications. But what’s actually the strongest medication for severe back pain? And more importantly, is it safe?
There’s no single "strongest" drug for everyone
Doctors don’t hand out the strongest painkiller like a trophy. What works for one person might be dangerous or useless for another. The strongest medication depends on your medical history, the cause of your pain, your risk of addiction, and how your body reacts to drugs.
For example, someone with a history of opioid addiction won’t be given morphine, even if it’s technically the most powerful. Someone with liver disease can’t take high-dose acetaminophen. The goal isn’t just to kill the pain-it’s to manage it safely over time.
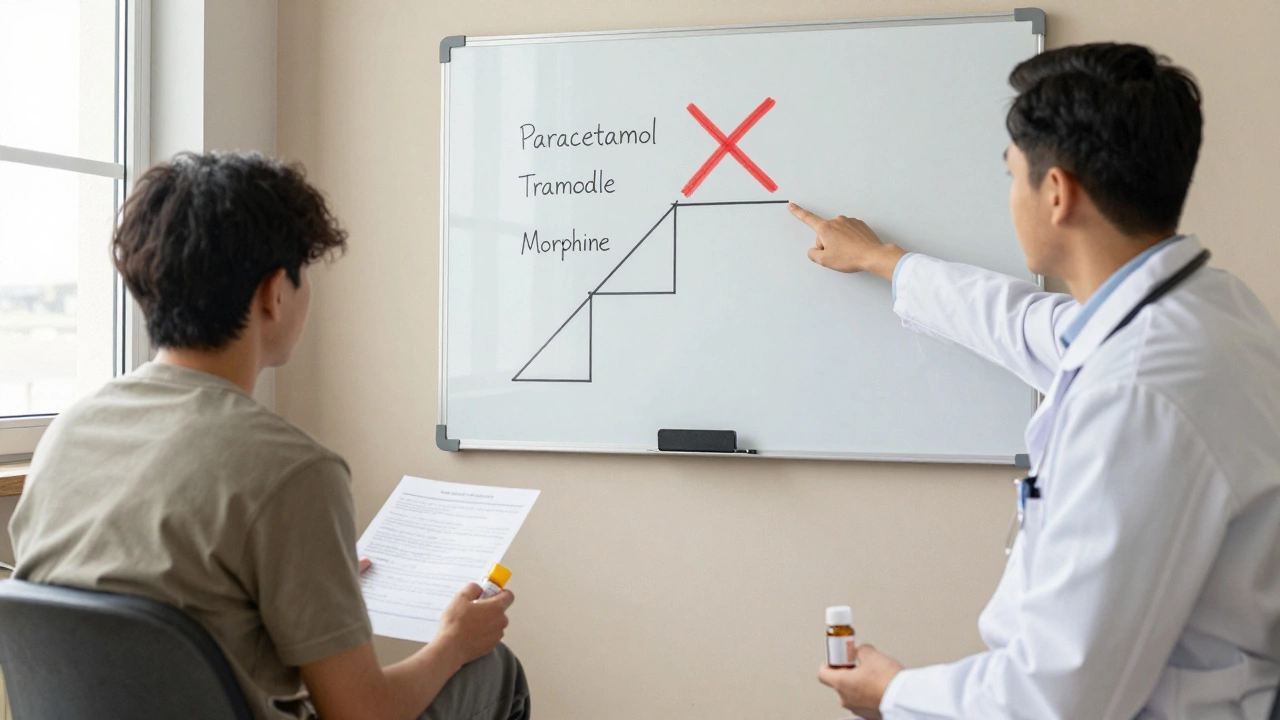
What counts as "strong"? The painkiller ladder
Medical guidelines use a step-by-step approach called the pain ladder. It starts with simple meds and climbs up to the most powerful options only when needed.
- Step 1: Paracetamol (acetaminophen) or NSAIDs like ibuprofen
- Step 2: Weak opioids like codeine or tramadol
- Step 3: Strong opioids like morphine, oxycodone, fentanyl, or hydromorphone
At Step 3, you’re talking about drugs that are tightly controlled. In Australia, these are Schedule 8 medications-meaning prescriptions are heavily monitored, and refills require special paperwork.
The top contenders for severe back pain
Here are the most potent medications actually prescribed for chronic, debilitating back pain:
- Morphine: The classic strong opioid. Used in hospitals and for end-stage pain. Oral morphine tablets or liquid can be prescribed for home use, but tolerance builds fast.
- Oxycodone: Often seen as more potent than morphine per milligram. Common brand names include OxyContin and Endone. It’s widely prescribed for chronic pain but has a high abuse potential.
- Fentanyl: Usually delivered as a patch (Duragesic) for long-term pain. It’s 80-100 times stronger than morphine. Only used when patients are already opioid-tolerant. Not for beginners.
- Hydromorphone (Dilaudid): Five to seven times stronger than morphine. Used when other opioids fail. Often given in clinics or hospice care.
- Tapentadol (Nucynta): A newer option that works like an opioid but also affects norepinephrine. It’s slightly less addictive than traditional opioids and sometimes used for neuropathic back pain.
These aren’t "magic bullets." They come with serious side effects: constipation, drowsiness, nausea, confusion, and a high risk of dependence. Many patients report that after a few months, they need higher doses just to feel the same relief.
Why stronger doesn’t mean better long-term
A 2023 study from the University of Sydney followed 1,200 patients with chronic low back pain over three years. Those on long-term opioids showed no better improvement in function or quality of life than those who used non-opioid treatments like physiotherapy and cognitive behavioral therapy.
What they did see? Higher rates of addiction, accidental overdoses, and hospital visits for side effects.
The American College of Physicians and the National Health and Medical Research Council (NHMRC) both recommend opioids only as a last resort-after trying:
- Physical therapy and targeted exercise
- Heat/cold therapy and massage
- Non-opioid medications (like gabapentin for nerve pain)
- Psychological support for pain-related anxiety or depression
Even if you’ve tried all that and still hurt, opioids aren’t a cure. They’re a tool to help you get through the worst days so you can do the real work: rebuilding strength and movement.
What about non-opioid alternatives?
Some of the most effective treatments for severe back pain aren’t opioids at all.
- Gabapentin and Pregabalin: These are anti-seizure drugs repurposed for nerve pain. If your back pain shoots down your leg (sciatica), they often work better than morphine.
- Duloxetine (Cymbalta): An antidepressant that also blocks pain signals in the spinal cord. Approved for chronic musculoskeletal pain.
- Topical lidocaine patches: For localized pain, these deliver numbing relief without systemic side effects.
- Corticosteroid injections: Injected directly into the spine or joint, they reduce inflammation. Not a cure, but can give you weeks or months of relief to start rehab.
One patient in Melbourne, 54, had failed three rounds of opioids before trying pregabalin and daily Pilates. Within six weeks, she went from needing a cane to walking 5 km. She’s still on medication-but now it’s a low-dose nerve pain drug, not a high-dose opioid.
When doctors say no to strong meds
Many GPs and pain specialists are now refusing to prescribe strong opioids for chronic back pain unless there’s a clear, short-term reason-like after major surgery or during cancer treatment.
Why? Because the risks outweigh the benefits for most people with long-term pain. The Australian Therapeutic Goods Administration (TGA) tightened rules in 2024, requiring doctors to register in the National Opioid Management Program and use prescription monitoring systems.
If your doctor says no to oxycodone, it’s not because they don’t care. It’s because they’ve seen too many people get trapped in a cycle of increasing doses, tolerance, and withdrawal.

What to do if you’re in severe pain right now
If your back pain is so bad you can’t move, don’t wait for a specialist. Go to an urgent care clinic or emergency department. They can:
- Rule out serious causes like spinal infection, fracture, or cauda equina syndrome
- Give you a short-term, supervised dose of strong pain relief
- Refer you to a multidisciplinary pain clinic
Don’t self-medicate with leftover pills from a friend or buy drugs online. Fake fentanyl patches are flooding the black market-and they’ve killed people.
Long-term strategy: Pain isn’t just a number
Severe back pain isn’t just about the intensity on a scale from 1 to 10. It’s about how it steals your life: missing work, losing sleep, avoiding hugs, feeling hopeless.
The strongest medication isn’t a pill. It’s a plan. A plan that includes:
- Physical rehab to rebuild core strength
- Psychological support to break the fear-pain cycle
- Activity pacing to avoid flare-ups
- Support groups to stop feeling alone
Many people who’ve been on opioids for years say the best day of their life wasn’t when they got their first prescription. It was the day they stopped chasing the next pill and started rebuilding their life.
Is morphine the strongest painkiller for back pain?
Morphine is one of the strongest opioids, but it’s not always the best choice. Fentanyl patches and hydromorphone are more potent per milligram. However, the "strongest" isn’t the most effective or safest. Doctors choose based on your body’s response, risk of addiction, and whether your pain is nerve-related or muscular.
Can I get oxycodone for chronic back pain?
Possibly, but it’s rare. In Australia, oxycodone is now only prescribed for chronic back pain if you’ve tried all other options and have a clear diagnosis. Even then, it’s usually limited to short-term use or very low doses. Most pain specialists won’t prescribe it unless you’re under their direct, ongoing care.
Are there safer alternatives to opioids for severe back pain?
Yes. Gabapentin and pregabalin work well for nerve pain like sciatica. Duloxetine helps with both pain and depression linked to chronic conditions. Topical creams, spinal injections, physiotherapy, and cognitive behavioral therapy are often more effective long-term than opioids-with far fewer risks.
What happens if I stop taking strong painkillers?
Stopping opioids suddenly can cause withdrawal: sweating, nausea, anxiety, insomnia, and muscle cramps. That’s why doctors taper doses slowly over weeks or months. Many people find that after withdrawal, their pain doesn’t get worse-it often improves because their nervous system resets. Physical therapy and psychological support make this transition easier.
Is it legal to buy strong painkillers online?
No. Buying opioids like oxycodone, fentanyl, or morphine online is illegal in Australia and extremely dangerous. Fake pills often contain fentanyl or other deadly substances. In 2024, Australian border authorities seized over 12,000 illicit opioid pills. Never risk your life for a pill from a website.
Next steps if you’re struggling
If you’re on strong painkillers and feel stuck, talk to your doctor about a pain management program. These programs combine physiotherapy, psychology, and medication review-not just more pills.
If you’re not on opioids but still in severe pain, ask for a referral to a pain specialist. They don’t just write scripts. They build plans.
Severe back pain is exhausting. But the strongest tool you have isn’t a prescription. It’s persistence. Finding the right team. And refusing to believe that pain has to be your whole life.





